“Understanding and Addressing Heart Blockage Symptoms"
A. Definition of Heart Blockages
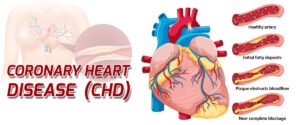
.Heart blockage symtoms refer to the obstruction or narrowing of blood vessels (arteries) that supply oxygen and nutrients to the heart muscle. These blockages typically result from the buildup of fatty deposits, cholesterol, and other substances, forming plaques within the arteries. Also the plaques accumulate, they can restrict or completely block the flow of blood, leading to reduced oxygen supply to the heart. This are a significant factor in cardiovascular diseases and potentially causing symptoms such as chest pain, shortness of breath, and fatigue. If left untreated, heart blockages can lead to serious complications, including heart attacks and other cardiac events. also, Early detection and appropriate management are crucial for preventing adverse outcomes and maintaining overall heart health.
B. Importance of Recognizing Heart blockage Symptoms
Recognizing
symptoms of heart blockages is of paramount importance in safeguarding
cardiovascular health.
1.
Timely Intervention: Early recognition allows for prompt medical intervention,
minimizing the risk of severe complications such as heart attacks and strokes
associated with untreated heart blockages.
2.
Prevention of Further Damage: Identifying symptoms facilitates timely
medical management, preventing further damage to the heart muscle and reducing
the likelihood of long-term complications.
3.
Improved Treatment Outcomes: Early intervention based on the
recognition of heart blockage symptoms improves the effectiveness of treatment. Also it can lead to better outcomes and a higher likelihood of successful recovery.
4.
Enhanced Quality of Life: To know the symptoms
promptly contribute to an improved quality of life for individuals with heart
blockages. Proper management can alleviate discomfort and enhance overall
well-being.
5.
Risk Stratification: The symptoms helps in assessing the severity of the
condition and stratifying the individual’s risk for cardiovascular events. This
information guides healthcare providers in tailoring appropriate treatment
plans.
6.
Patient Empowerment: Knowledge of heart blockage symptoms also empowers individuals to
take an active role in their health. Recognizing warning signs encourages them
to seek timely medical attention, fostering a sense of control over their
well-being.
7.
Reduction of Emergency Situations: and Awareness of symptoms
reduces the likelihood of sudden, severe cardiac events. This, in turn,
minimizes the need for emergency interventions, lowering healthcare costs and
improving resource utilization.
8.
Public Health Impact: Public awareness of heart blockage symptoms contributes to a
broader public health impact. Also, Educational campaigns and initiatives can lead to
healthier lifestyles and a reduction in the overall burden of cardiovascular
diseases.
Common symptoms of heart blockage symptoms
Common symptoms of heart blockages typically manifest due to
reduced blood flow to the heart muscle, leading to oxygen deprivation and
compromised cardiac function. These symptoms, often referred to as “heart
blockage symptoms,” include:
Chest Pain (Angina): Chest pain or discomfort, often characterized by pressure,
squeezing, or tightness in the chest.
Variations in Pain Intensity: Pain may vary from mild to severe
and may radiate to the neck, jaw, shoulders, arms, or back.
Shortness of Breath (Dyspnea): Difficulty breathing or feeling
breathless, especially during physical exertion or when lying flat.
Occurrence During Physical Activity: Breathlessness may worsen
with exertion as the heart struggles to meet the increased demand for
oxygen-rich blood.
Fatigue: Feeling unusually tired or fatigued, even after adequate rest or
minimal physical activity.
Impact on Daily Activities: Fatigue may interfere with daily
tasks, leading to decreased productivity and reduced quality of life.
Dizziness or Light-headedness: Sensation of light-headedness,
dizziness, or feeling faint, often accompanied by a sense of impending loss of
consciousness.
Palpitations: Awareness of abnormal heartbeats, such as rapid, fluttering, or
pounding sensations in the chest.
Fluttering or Pounding Sensation: Palpitations may be
intermittent or persistent and may cause discomfort or anxiety.
Swelling: Edema in Legs, Ankles, or Abdomen; due to Accumulation of fluid
in the lower extremities or abdomen, leading to swelling, bloating, or a
feeling of heaviness.
Fluid Retention Due to Heart Dysfunction: Reduced cardiac output
can cause fluid buildup in the body’s tissues, resulting in swelling.
Less Common Symptoms of heart blockages
Nausea or Vomiting: Feeling of nausea or actual vomiting, which may not be directly
associated with digestive issues but could be a result of reduced blood flow
compromising the digestive system.
Cold Sweats: Experiencing clammy or cold sweats that are not attributed to
external factors, such as high temperatures or physical exertion.
Jaw, Neck, or Back Pain: Pain, discomfort, or pressure in the jaw,
neck, or back, which may radiate from the chest and could be mistaken for
muscle pain.
Indigestion or Heartburn: Unexplained indigestion or persistent
heartburn that is not relieved by antacids or dietary changes.
Sudden Weakness: Sudden onset of weakness or unexplained fatigue, unrelated to
physical activity or lack of sleep.
These less common symptoms may be subtle, intermittent, or
easily attributed to other non-cardiac factors. Individuals experiencing any of
these symptoms, with other warning signs, should consult with a healthcare
professional for a thorough evaluation. Early detection and intervention can
significantly improve outcomes and prevent more severe complications associated
with heart blockages.
When to Seek Medical Help
Knowing when to seek medical help for suspected heart blockages is crucial for timely intervention and preventing potentially life-threatening complications. Here are some guidelines for when to seek medical assistance:
1. Persistent Chest Pain or Discomfort: One who experience persistent chest pain or discomfort, especially if it spreads to your arm, neck, jaw, or back, seek medical attention immediately. This could be a sign of a heart attack or unstable angina.
2. Shortness of Breath: Patient with sudden or severe shortness of breath, especially if it’s accompanied by chest pain, dizziness, or lightheadedness, seek medical help promptly. This could indicate a heart-related issue requiring urgent
evaluation.
3. Unexplained Fatigue or Weakness: If you feel unusually tired or weak, especially if it’s sudden or severe, and it’s not relieved by rest, consult a healthcare provider. Fatigue can be a symptom of heart failure or reduced cardiac function.
4. Dizziness or Fainting: If anyone experience frequent or severe dizziness, lightheadedness, or fainting spells, especially if they occur suddenly and without warning, seek medical attention. and These symptoms could be related to abnormal heart rhythms or inadequate blood flow to the brain.
5. Palpitations or Irregular Heartbeat: The frequent palpitations or an irregular heartbeat, especially if it’s accompanied by chest discomfort, shortness of breath, or fainting, it’s essential to see a doctor. These symptoms may indicate an arrhythmia or other cardiac issue.
6. Swelling in the Legs, Ankles, or Abdomen: If patient notice sudden or significant swelling in your legs, ankles, or abdomen, especially if it’s accompanied by other symptoms such as shortness of breath or fatigue, seek
medical help. This could indicate heart failure or fluid retention due to reduced cardiac function.
7. Previous History of Heart Disease: If you have a history if heart disease, heart attacks, or other cardiac issues, and you experience any new or worsening symptoms, it’s important to contact your healthcare provider promptly for evaluation and management.
Diagnosis and testing for heart blockage symptoms
It
involves a series of medical evaluations and procedures aimed at identifying
the underlying cause of the symptoms and assessing the severity of the
condition. Here are some common diagnostic methods used:
1.
Physical Examination: A healthcare provider will conduct a thorough physical
examination, including checking your vital signs, listening to your heart and
lungs, and assessing any visible signs of heart disease such as swelling in the
legs or ankles.
2.
Electrocardiogram (ECG or EKG): An ECG is a
non-invasive test that records the electrical activity of the heart. It can
detect abnormal heart rhythms, signs of previous heart attacks, and other
cardiac abnormalities that may be associated with heart blockages.
3.
Echocardiogram: An echocardiogram uses sound waves to create images of the
heart’s structure and function. It can help assess the pumping function of the
heart, identify areas of reduced blood flow, and detect structural
abnormalities such as heart valve problems or heart muscle dysfunction.
4. Stress Test: A stress test, also known as a treadmill test or exercise test, evaluates how your heart responds to physical activity. It involves walking on a treadmill or riding a stationary bike while your heart rate and ECG are monitored. This test can help identify heart blockages that may become more apparent during exercise when the heart’s demand for oxygen-rich blood increases.
5.
Blood Tests: Blood tests may be conducted to measure levels of certain
substances in the blood that can indicate heart damage or increased risk of
heart disease, such as cardiac enzymes, lipid profiles (cholesterol levels),
and markers of inflammation.
Shanikrupa
Heartcare provides a diagnostic tests and procedures help healthcare providers
accurately diagnose heart blockages, determine the extent of the blockages,
assess overall cardiac function, and guide treatment decisions.
Living with Heart Blockages
Living with heart blockages requires a proactive approach. Also, lifestyle to minimize heart blockage symptoms.
1. Medication Adherence: This may include medications to manage symptoms, control blood pressure, lower cholesterol levels, prevent blood clots, or improve heart function.
2. Healthy Lifestyle Choices: Adopting a heart-healthy lifestyle can significantly impact your quality of life and long-term health.
This includes:
· Following a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats while limiting sodium, saturated fats, and refined sugars.
· Engaging in regular physical activity, as recommended by your healthcare provider. Exercise helps improve cardiovascular health, manage weight, and reduce stress.
· Quitting smoking and avoiding exposure to second hand smoke, as smoking increases the risk of heart disease and worsens heart blockages.
· Limiting alcohol intake, as excessive alcohol consumption can contribute to high blood pressure, irregular heart rhythms, and other cardiac issues.
3. Monitoring Symptoms: Keep track of your blood pressure, heart rate, and any other relevant indicators as advised by your healthcare provider.
4. Managing Stress: Practice relaxation techniques such as deep breathing, meditation, yoga, or hobbies that you enjoy.
5. Regular Follow-Up Care: Attend scheduled follow-up appointments with your healthcare provider to monitor your condition, adjust treatment plans as needed.
6. Support Network: Surround yourself with a supportive network of family, friends, and healthcare professionals who can provide encouragement, assistance, and guidance as you navigate living with heart blockages.
7. Cardiac Rehabilitation: These programs typically include supervised exercise, education on heart-healthy lifestyle choices, and support to help you recover from heart-related issues and improve overall cardiovascular health.
Heart-Healthy Foods
Heart-healthy foods are nutrient-rich options that promote
cardiovascular health and help reduce the risk of heart disease, including
heart blockages. Incorporating these foods into your diet can support overall
heart health.
·
Fruits and Vegetables: Rich in vitamins, minerals, antioxidants, and fiber, fruits and
vegetables are essential components of a heart-healthy diet. Aim to include a
variety of colorful options such as berries, citrus fruits, leafy greens,
carrots, bell peppers, and broccoli.
·
Whole Grains: Choose whole grains over refined grains to increase fiber intake
and improve heart health. Examples oats, quinoa, brown rice, whole wheat bread,
and barley.
· Healthy Fats: Incorporate sources of
healthy fats, such as monounsaturated and polyunsaturated fats, into your diet.
Good sources of healthy fats include avocados, nuts, seeds, olive oil, and
fatty fish like salmon, mackerel, and trout.
· Lean Protein: Choose lean cuts of
poultry (without skin), fish, legumes (beans, lentils, chickpeas), tofu, and
low-fat dairy products.
·
Plant-Based Proteins: Incorporate plant-based protein sources into your diet, such as
beans, lentils, tofu, tempeh, and edamame. These foods are rich in fiber,
vitamins, and minerals and can help lower cholesterol levels and reduce the
risk of heart disease.
· Low-Fat Dairy: Choose low-fat or
fat-free dairy products to reduce saturated fat intake while still obtaining
essential nutrients like calcium and vitamin D.
·
Nuts and Seeds: Enjoy nuts and seeds in moderation as part of a heart-healthy
diet. They are rich in healthy fats, fiber, protein, vitamins, and minerals.
Examples include almonds, walnuts, flaxseeds, chia seeds, and pumpkin seeds.
· Herbs and Spices: Flavor your meals with
herbs and spices instead of salt to reduce sodium intake and support heart
health.
· Limit Sodium and Added
Sugars: Reduce
intake of processed and packaged foods high in sodium and added sugars, as they
can contribute to high blood pressure, inflammation, and heart disease.
Exercise Guidelines for Heart Health
Exercise is a crucial component of maintaining heart health
and reducing the risk of heart disease, including heart blockages
·
Aerobic Exercise: Aim for at least 150
minutes of moderate-intensity aerobic exercise or 75 minutes of
vigorous-intensity aerobic exercise per week, spread out over several days.
·
Types of Exercise: Choose activities that
elevate your heart rate and increase breathing, such as walking, jogging,
cycling, swimming, dancing, or using cardio machines like treadmills or
ellipticals.
·
Moderate-intensity exercise should make
you feel warm and slightly out of breath but still able to carry on a
conversation. Vigorous-intensity exercise should make you breathe harder and
faster, making it difficult to carry on a conversation.
·
Duration and Frequency: Aim for at least
30 minutes of aerobic exercise on most days of the week. If you’re unable to
exercise for 30 minutes at a time, break it up into shorter sessions throughout
the day, such as three 10-minute sessions.
·
Warm-Up and Cool Down: Always start your
exercise session with a 5-10 minute warm-up to prepare your body for activity
and gradually increase your heart rate.
·
Strength Training: Incorporate strength
training exercises at least two days per week, targeting major muscle groups
such as the legs, arms, chest, back, and core. Strength training helps improve
muscle strength, endurance, and bone density, which are important for overall
health and function.
·
Flexibility and Balance: Include
flexibility exercises such as yoga or stretching to improve joint mobility and
range of motion.
·
Listen to Your Body: Pay attention to how
your body feels during exercise and adjust the intensity or duration as needed
·
Stay Hydrated: Drink plenty of water
before, during, and after exercise to stay hydrated, especially in hot weather
or during intense workouts.
FAQs (Frequently Asked Questions)
A. Can heart blockages be reversed?
Adopting a heart-healthy lifestyle, exercising regularly, quitting smoking, and managing stress, can improve heart health and reduce the risk of complications.
B. What are the risk factors for heart blockages?
Risk factors for heart blockages include high blood pressure, high cholesterol levels, smoking, diabetes, obesity, physical inactivity, unhealthy diet, family history of heart disease, age, and stress.
C. Is family history a significant factor in heart blockages?
Yes, family history plays a significant role in determining the risk of heart blockages. It’s essential to be aware of your family history and discuss it with your doctor to assess your risk and take appropriate preventive measures.
D. Can heart blockages occur in younger individuals?
Heart blockages are more common in older adults, they can occur in younger individuals, especially those with risk factors such as a family history of heart disease, unhealthy lifestyle habits, or underlying medical conditions like diabetes or high blood pressure
E. How often should individuals with heart blockages undergo medical check-ups?
Generally, individuals with heart blockages may require regular monitoring, including follow-up appointments with cardiologists, screenings for heart-related issues, and tests to assess heart function and blood vessel health.
F. Can stress contribute to heart blockages?
Yes, chronic stress can contribute to the development and progression of heart blockages and other cardiovascular problems. Stress can lead to unhealthy coping mechanisms such as overeating, smoking, or physical inactivity, which can increase the risk of heart disease.
G. Are their alternative therapies for managing heart blockages?
While lifestyle changes and medications are the primary treatments for managing heart blockages, some alternative therapies may complement conventional treatments, promote heart health. Chelation therapy, EECP
treatment, dietary supplements (e.g., omega-3 fatty acids, Coenzyme Q10), acupuncture, massage therapy, relaxation techniques (e.g. yoga, meditation).